Virginia has, at the same time, a behavioral healthcare crisis, and a record-breaking $2.6 billion budget surplus. Flush in money, our elected leaders seem to want to see private healthcare providers take the lead on taking care of that little behavioral healthcare issue.
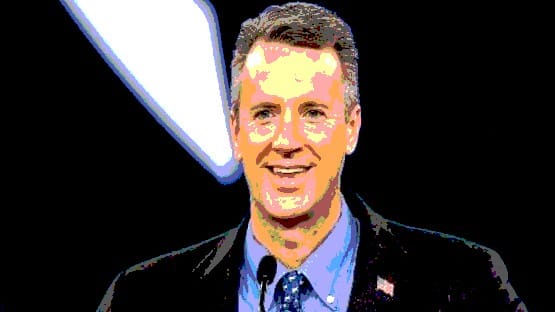
“Even as our hospitals serve on the frontlines of the COVID-19 pandemic, they are simultaneously confronting a behavioral health care crisis that has gone from bad to worse. The number of individuals seeking behavioral health care treatment has steadily increased amidst the ongoing COVID-19 pandemic. This has occurred against the backdrop of a diminished network of community-based services and a growing shortage in capacity related to workforce in state[1]run and community-based facilities,” Virginia Hospital & Healthcare Association President and CEO Sean Connaughton wrote in a letter addressed to legislative leaders dated July 21.
“The most urgent action the Commonwealth can take is directing large-scale resources to recruit and retain workforce in the behavioral health care sector. This will enable behavioral health care facilities to maximize bed capacity, as there are currently many beds inaccessible and offline specifically due to lack of staff,” Connaughton wrote in the letter, which notes the burden being put on acute-care hospitals to provide behavioral health services that they’re not necessarily designed to be able to offer.
“The acute care hospital system in the Commonwealth is available 24/7/365 and provides for the emergency and inpatient medical needs of individuals experiencing a behavioral health care crisis, and their respective communities. The role of these hospitals is to evaluate, stabilize, treat, and as needed for efficient and safe discharge, refer individuals to appropriate community-based services. Acute care hospitals are primarily intended to provide short-term care,” Connaughton wrote.
And yet, Virginia hospitals “consistently provide care to the overwhelming majority of behavioral health care and substance use/misuse patients in inpatient settings,” according to Connaughton, with approximately 92 percent of the behavioral healthcare and substance use/misuse patient discharges each year coming from private hospitals.
“The average length of stay for inpatient behavioral health care patients in private hospitals is increasing and is now more than seven days, nearly eight percent higher than it was just two years ago. What this means is that fewer patients are occupying finite acute care hospital bed capacity for longer periods of time,” Connaughton wrote.
The VHHA is offering to help the state deal with another crisis in the form of workforce staffing shortages that forced the temporary closure of admissions at five state hospitals on July 9 by opening 58 psychiatric beds statewide, but the state, according to Connaughton, wants hospitals to do more.
“The state’s true desire is for acute care hospitals to handle more patients who are medically complex, have a history of high aggression or behavioral challenges, have intellectual or developmental disabilities, or are geriatric patients with a primary diagnosis of dementia. An acute care setting is not the appropriate venue for providing optimal and safe care to meet the needs of these patients. Practically speaking, placing patients in need of long-term care in acute care hospitals is generally not feasible and not clinically appropriate,” Connaughton wrote.
“Such an action would also reduce overall treatment capacity by leading to extended psychiatric bed occupancy, continue workforce flight due to excessively stressful work conditions and deprive other patients in urgent need the opportunity for treatment. Taking this approach will not solve the state’s problems and will limit private hospitals’ ability to serve individuals in their respective communities,” Connaughton wrote.
In place of another stop-gap measure, Connaughton suggests that “(a)dditional consideration should be given to a more thoughtful, evidence-based, proactive strategy that prioritizes sustainable resource allocation and reimbursement parity.”
“Behavioral health care has been widely acknowledged as being under-resourced, siloed and uncoordinated, and impacted by increased regulatory requirements and financial pressures for decades,” Connaughton wrote.
“As we noted in our July 11 letter, ‘the current budget surplus, along with the infusion of funding from the federal government via the American Recovery Plan Act (ARPA) for COVID-19 related recovery efforts enables the Commonwealth to provide crucial funding to behavioral health care providers. This funding is imperative to ensure those in need of behavioral health care are provided access to the appropriate services in the proper environment.’ Given the resources presently available, this is a once-in-a-generation opportunity for the Commonwealth to invest in strengthening the behavioral health care system,” Connaughton wrote.
Story by Chris Graham